Blind Pimples: How to Get Rid of Those Hard, Stubborn Bumps Under the Skin
Tired of those painful, hidden pimples that just won’t go away? You’re not alone. These hard bumps, often called blind pimples, are a common skin concern that can be tricky to treat.
As a dermatologist, I see at least five patients a week struggling with these deep pimples that lurk under the skin’s surface. They don’t pop like regular pimples and can last for weeks or even months.
In this article, we’ll cover what blind pimples are, what causes them, and most importantly—how to treat and prevent them effectively.
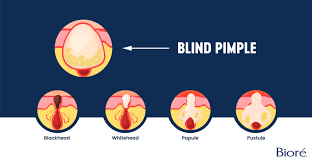
What Are Blind Pimples?
Blind pimples are hard, inflamed bumps under the skin that don’t have a visible whitehead or blackhead. These bumps can be painful, red, and swollen. They’re deep and feel like small knots beneath the surface.
Unlike surface pimples, these are rooted deep in the skin and can become nodular acne if they are larger than 1 cm. Blind pimples can sometimes evolve into epidermal inclusion cysts (EICs) if not managed correctly.
Because they never “come to a head,” people often try to pop or squeeze them, which only worsens inflammation and increases the chance of scarring or infection.
Types of Hard Bumps Under the Skin
Not all bumps under the skin are blind pimples. Here’s a breakdown of what they could be:
1. Inflammatory Acne Lesions
These include papules and nodules. Papules are less than 1 cm, while nodules are larger. Both are red, painful, and don’t contain visible pus.
2. Non-Inflammatory Acne Lesions
These are comedones—like whiteheads and blackheads. They’re closer to the skin surface and typically not painful.
3. Blind Pimples (Papules)
Blind pimples fall into the inflammatory category but have no visible head. They form deep under the skin and can be painful to the touch.
4. Epidermal Inclusion Cysts (EICs)
These are slow-growing, firm lumps under the skin filled with keratin. They often release a foul-smelling discharge when ruptured.
5. Sebaceous Cysts
These are often confused with EICs but are essentially the same thing under a different name.
6. Milia
Milia are small, white, seed-like bumps made of keratin. They are not true pimples and usually appear on the cheeks and around the eyes.
What Causes Blind Pimples?
Blind pimples are caused by clogged pores. When dead skin cells, sebum (oil), and bacteria become trapped inside the pore, the area becomes inflamed.
Here are the common triggers:
Hormonal fluctuations, especially during menstruation or puberty
Excess oil production from overactive sebaceous glands
Skincare products that clog pores
Not cleansing the face properly or regularly
Poor diet and high sugar intake
Stress and lack of sleep
Genetic predisposition
Characteristics of Blind Pimples
No visible whitehead or blackhead
Painful and red
Feels like a hard knot under the skin
May grow in size over several days
Skin may appear slightly swollen or warm
Because they form deep below the surface, these pimples don’t pop and take longer to heal than other types of acne.
How to Prevent Blind Pimples
Preventing blind pimples starts with consistent skincare and healthy habits. Here are dermatologist-approved prevention tips:
1. Cleanse Twice Daily
Use a cleanser tailored to your Baumann Skin Type to remove oil, dirt, and bacteria. Take the skin type quiz to determine the right routine for you.
2. Use Acne-Fighting Ingredients
Salicylic acid and benzoyl peroxide help keep pores clear and reduce acne-causing bacteria.
3. Avoid Pore-Clogging Products
Stay away from moisturizers or cosmetics labeled “comedogenic.”
4. Incorporate Retinoids
Retinoids help speed up cell turnover, preventing clogs that cause blind pimples.
5. Exfoliate Weekly
Use a gentle chemical exfoliant like a BHA mask once a week to remove dead skin cells.
6. Keep Your Environment Clean
Change pillowcases regularly, clean your phone screen, and avoid touching your face.
7. Watch Your Diet
Reduce sugar and greasy foods. A clean diet can help reduce inflammation and sebum production.
Effective Home Remedies for Blind Pimples
1. Warm Compress
Apply a warm compress for 10–15 minutes, 2–3 times daily. It improves blood flow and may help bring the pimple to the surface.
2. Tea Tree Oil
Dilute with a carrier oil and apply with a cotton swab. Its antibacterial properties help reduce bacteria and inflammation.
3. Aloe Vera
Apply pure aloe vera gel to calm redness and irritation.
4. Honey or Apple Cider Vinegar
These have antibacterial and anti-inflammatory properties that help calm the skin.
Over-the-Counter Treatments
Look for products containing:
Benzoyl Peroxide – Kills acne-causing bacteria.
Salicylic Acid – Penetrates pores to dissolve oil and dead skin.
Retinol Serums – Help with skin turnover and pore decongestion.
One standout product is SkinCeuticals Blemish + Age Defense, which contains salicylic acid and was found in studies to be as effective as prescription Benzaclin.
Sensitive skin types may need to introduce salicylic acid and retinol slowly to avoid irritation.
Prescription Treatments for Blind Pimples
1. Topical Retinoids
Such as tretinoin, adapalene, or tazarotene. These speed up skin turnover and bring blind pimples to the surface faster.
2. Antibiotic Creams or Pills
These fight bacterial infection and inflammation when breakouts are widespread.
3. Hormonal Therapies
Birth control pills or spironolactone may be prescribed for hormone-related acne.
4. Corticosteroid Creams
Prescription steroid creams like triamcinolone can reduce inflammation, but only for short-term emergencies.
Important Note: Long-term steroid use can cause side effects like skin thinning, stretch marks, spider veins, or steroid acne.
Professional Treatments for Blind Pimples
1. Corticosteroid Injections
The fastest way to shrink a blind pimple overnight. A dermatologist injects a small amount of steroid directly into the pimple.
2. Chemical Peels
These help reduce acne, improve skin texture, and speed up healing by removing dead skin layers.
3. Laser and Light Therapy
Photodynamic and laser treatments can target oil production and bacteria but are usually used for long-term acne management—not emergency pimple relief.
What About Extractions?
Blind pimples should not be extracted. Since they don’t have a head or pus pocket, extraction can cause trauma and even turn them into cysts.
Only a dermatologist should decide if a bump is ready for extraction or needs a different treatment.
Dos and Don’ts for Blind Pimples
Do:
Use targeted acne treatments
Keep your hands and face clean
Follow a consistent skincare routine
Visit a dermatologist for large or painful lesions
Don’t:
Pick or squeeze the pimple
Use harsh scrubs or exfoliants
Skip sunscreen (some acne treatments increase sensitivity)
Use heavy oils or comedogenic creams
When to See a Dermatologist
You should see a dermatologist if:
Pimples persist for more than a few weeks
You have frequent or painful blind pimples
At-home treatments don’t work
You’re developing scarring or discoloration
A dermatologist can create a personalized treatment plan and may recommend prescription medications or procedures.
Final Thoughts: Take Control of Your Skin
Blind pimples are frustrating, painful, and often slow to heal. But with the right skin care routine, targeted products, and habits, they can be managed—and even prevented completely.
Take the Baumann Skin Type Quiz to determine the best medical-grade skincare products tailored for your skin.
Say goodbye to blind pimples for good—without picking or scarring.


